The New Science of Weight Management: Why Health Should Be the Real Goal

In the relentless quest for weight loss, society has often overlooked the most vital aspects of true health and well-being. The narrative around weight loss has long been dominated by simplistic equations—calories in versus calories out—and narrow ideals that prize thinness above true metabolic integrity. As a result, we have reduced our health aspirations to chasing ever-smaller numbers on a scale, believing that a shrinking body automatically equates to a healthier one. Scales become the ultimate judges of success, calories are demonized, and bodies are measured solely in terms of appearance rather than function, resilience, or vitality.
But beneath this cultural obsession lies a deeper and more revolutionary truth—one that challenges the conventional paradigm. Real, lasting, and meaningful weight management is not about deprivation; it’s about preservation. It’s about holding onto what matters most—muscle, bone, mitochondrial health, hormonal harmony, and cognitive clarity—while shedding excess fat and inflammation. It’s about cultivating a system that’s robust and vibrant, not simply lighter. This shift in mindset reframes weight loss as a process of gaining strength, longevity, and inner stability—not just losing weight for aesthetics or short-term gratification.
Far too many people have embarked on weight loss journeys only to end up depleted—physically, emotionally, and metabolically. We must ask ourselves: are we pursuing health, or simply thinness? Sustainable weight management is about optimizing every system in the body, not starving them. The real prize isn’t dropping sizes—it’s gaining strength, resilience, and an enduring quality of life.
Lean Mass: The Metabolic Gold
Muscle is not a luxury; it’s a necessity. In the evolving conversation around weight loss, preserving lean body mass—particularly skeletal muscle—has emerged as a critical yet often neglected priority. Beyond aesthetics or performance, lean mass is fundamentally tied to overall metabolic health, insulin sensitivity, immune resilience, and even mental vitality. Muscle tissue is a metabolically active organ that not only consumes energy at rest but also acts as a powerful regulator of systemic glucose levels, inflammation, and hormonal balance. As we age, the gradual loss of muscle mass—known as sarcopenia—can quietly shift the balance from healthy weight loss to a cascade of health challenges including insulin resistance, frailty, increased fall risk, and accelerated biological aging [1].
When people pursue aggressive calorie restriction or over-exercise without strategic support, the body often breaks down muscle to meet its energy demands. This muscle loss weakens not just physical strength but the very foundation of metabolic health. Lean muscle functions as a reservoir for glucose and amino acids, providing both energy and essential substrates during times of stress or caloric deficit [2]. Just as importantly, muscle acts as an endocrine organ, releasing beneficial signaling molecules called myokines during contraction. These myokines exert anti-inflammatory, anti-diabetic, and even anti-tumor effects, helping the body maintain homeostasis across systems—from the brain to the liver and immune system [3]. Thus, muscle isn’t just something to “tone up”—it’s an essential, active player in the body’s weight regulation machinery.
To protect muscle during weight loss, several interventions must work in tandem. First and foremost is resistance training, ideally performed at least three to four times per week. Compound movements like squats, deadlifts, and push-pull sequences activate large muscle groups and stimulate protein synthesis, which not only prevents loss but may build new muscle even in a calorie deficit. Second, adequate protein intake is crucial—aiming for 1.2 to 2.0 grams of protein per kilogram of body weight per day is a clinically supported benchmark [4]. This becomes especially important with age, when anabolic resistance increases the protein requirements for maintaining muscle tissue. Supplementation with branched-chain amino acids (BCAAs), particularly leucine, can help preserve lean mass during weight loss and intermittent fasting, providing targeted stimulation of mTOR for muscle synthesis without excessive overall calories [5].
Beyond protein and training, strategic support with nutrients like magnesium citrate can improve muscular recovery and reduce post-exercise inflammation.
Similarly, riboflavin (B2) and niacin (B3), taken in higher therapeutic doses, can enhance mitochondrial efficiency within muscle cells—optimizing ATP production, reducing oxidative stress, and boosting endurance capacity. For individuals pursuing advanced mitochondrial support, compounds like methylene blue are emerging as adjuncts that enhance electron transport and reduce cellular fatigue, potentially preserving muscle function during caloric restriction.
Resveratrol, a polyphenol found in red grapes and berries, also supports lean mass by activating the SIRT1-AMPK pathway, which indirectly inhibits mTOR overactivation while enhancing mitochondrial biogenesis and insulin sensitivity. Its mild mTOR modulation may allow for fat loss while preserving muscle, especially in those undergoing intermittent fasting or ketogenic nutrition. Moreover, resveratrol’s anti-inflammatory and antioxidant properties help blunt catabolic signals that can otherwise accelerate muscle breakdown in calorie-deficit states.
Another crucial yet underappreciated tool in maintaining lean mass during weight management is pregnenolone, the master neurosteroid and precursor to hormones like DHEA, progesterone, testosterone, and cortisol. During extended stress, fasting, or caloric restriction, the body may shunt hormone production toward cortisol at the expense of anabolic and neuroprotective pathways—a process known as pregnenolone steal. Supplementing with low physiological doses of pregnenolone may help buffer against this depletion, promoting more balanced endocrine signaling. This can support muscle protein synthesis indirectly by stabilizing testosterone and DHEA levels, while also improving cognitive clarity and motivation—factors often compromised during prolonged dieting. Pregnenolone’s ability to modulate GABA and NMDA receptors also contributes to better sleep and recovery, both of which are essential for muscle preservation and repair.
Bone Density: The Silent Strength
Bone may seem inert and structural, but in truth, it is a dynamic, living tissue that communicates constantly with the rest of the body. In the context of weight loss, bone health is often an afterthought—but it shouldn’t be. Weight loss that leads to the erosion of bone mass can quietly accelerate biological aging, especially in vulnerable populations such as postmenopausal women, individuals on restrictive diets, and the elderly [6]. The consequences aren’t merely cosmetic or mobility-related; reduced bone density increases the risk of fractures, chronic pain, and long-term disability. Moreover, it often happens silently, without overt symptoms, until a major injury reveals the underlying fragility.
Emerging science shows that the relationship between bone and metabolism is far more intimate than previously understood. Bone is not just scaffolding—it’s a metabolically active endocrine organ. Hormones like osteocalcin, secreted by bone-forming osteoblasts, have systemic effects, including enhancing insulin sensitivity, increasing testosterone production, and improving mitochondrial function [7]. This means that bone health is intertwined with the very processes we seek to optimize during weight loss: hormonal balance, energy production, and metabolic control. Compromising bone in the pursuit of fat loss may paradoxically impair the body’s ability to maintain that loss.
To preserve and build bone during weight loss, several strategies should be prioritized. Weight-bearing exercises—especially resistance training, yoga, hiking, and bodyweight movements—stimulate the mechanical loading needed to trigger bone remodeling. Unlike cardio alone, resistance exercises apply specific stress to bones, prompting adaptive strengthening and improved density over time. This is essential not only for maintaining skeletal strength but also for enhancing joint integrity and posture.
Nutritional support is equally vital. Vitamin D3 enhances calcium absorption, while vitamin K2 helps shuttle calcium into bones and away from arteries—an often-overlooked nuance in preventing vascular calcification. Among minerals, magnesium citrate stands out due to its superior bioavailability and dual action: it supports both bone mineralization and muscle relaxation, making it invaluable during weight loss regimens that include increased physical training [8]. Magnesium is also involved in over 300 enzymatic processes, many of which influence bone turnover, hormonal balance, and inflammation regulation.
Tracking progress through periodic DEXA scans is a smart and often underutilized strategy [9]. DEXA not only provides a snapshot of bone density but also differentiates between fat mass and lean mass, offering a more complete picture of body composition. For those serious about sustainable, health-promoting weight loss, knowing what’s being lost—fat, muscle, or bone—can be the difference between transformation and regression. Prioritizing bone health isn’t just about preventing fractures; it’s about safeguarding the silent strength that upholds metabolic vitality, mobility, and longevity.
The Role of Inflammation
Fat is not merely passive storage for excess calories—it is a hormonally active, immunologically significant organ system that communicates continuously with the rest of the body. In particular, visceral fat, the type that surrounds internal organs, acts as an endocrine organ that secretes a range of pro-inflammatory cytokines, including TNF-α (tumor necrosis factor alpha) and IL-6 (interleukin-6). These inflammatory mediators interfere with insulin receptor signaling, promoting systemic insulin resistance, dysregulated glucose metabolism, and chronic low-grade inflammation—hallmarks of metabolic syndrome and type 2 diabetes [10].
This persistent inflammatory milieu does more than just stall weight loss efforts; it actively degrades health on multiple fronts. Chronic inflammation damages the endothelial lining of blood vessels, accelerating the development of atherosclerosis and increasing cardiovascular risk. It also contributes to neuroinflammation, impairing cognitive performance, mood, and increasing the risk of neurodegenerative diseases such as Alzheimer’s. On a cellular level, inflammation directly impairs mitochondrial function, decreasing energy production, increasing reactive oxygen species (ROS), and promoting fatigue, aging, and metabolic inefficiency. Thus, inflammation is not just a symptom but a central driver of disease and weight regulation failure.
The solution lies in comprehensive inflammation control—not through suppressing the immune system, but by retraining and nourishing it through strategic interventions. A whole-food, anti-inflammatory diet is foundational. This includes generous intake of polyphenol-rich fruits and vegetables, fiber to feed beneficial gut bacteria, and omega-3 fatty acids from sources like walnuts, and fatty fish [11]. These nutrients help reduce the production of pro-inflammatory mediators and increase anti-inflammatory counterparts like IL-10 and adiponectin.
Beyond nutrition, lifestyle strategies such as mindful stress reduction, high-quality sleep, and intermittent fasting help rebalance the hypothalamic-pituitary-adrenal (HPA) axis and reduce cortisol-mediated inflammation [12]. Even moderate exercise can lower C-reactive protein (CRP) levels and stimulate anti-inflammatory myokines from skeletal muscle. These habits, when practiced consistently, form the foundation of an anti-inflammatory lifestyle.
Targeted supplementation provides another layer of support. Curcumin, the active compound in turmeric, inhibits the NF‑κB pathway, a master regulator of inflammation. Ginger, with its natural COX-2-inhibiting properties, also offers synergistic anti-inflammatory action. Of special interest is resveratrol, a plant-derived polyphenol that activates sirtuins, particularly SIRT1, which play a critical role in modulating inflammatory responses and mitochondrial function [13]. Resveratrol not only blunts the cytokine storm associated with visceral fat but also helps recalibrate the body’s inflammatory thermostat at a molecular level. Its dual role in mitochondrial protection and inflammatory modulation makes it an ideal candidate for individuals looking to reduce fat mass without compromising metabolic resilience.
By recognizing and targeting inflammation as a root cause—not just a side effect—of weight challenges, we lay the groundwork for more sustainable and meaningful health outcomes. Inflammation is not just a fire to be put out; it is a biological signal that, when properly interpreted and addressed, can guide us toward deeper healing, improved vitality, and longer-lasting weight regulation.
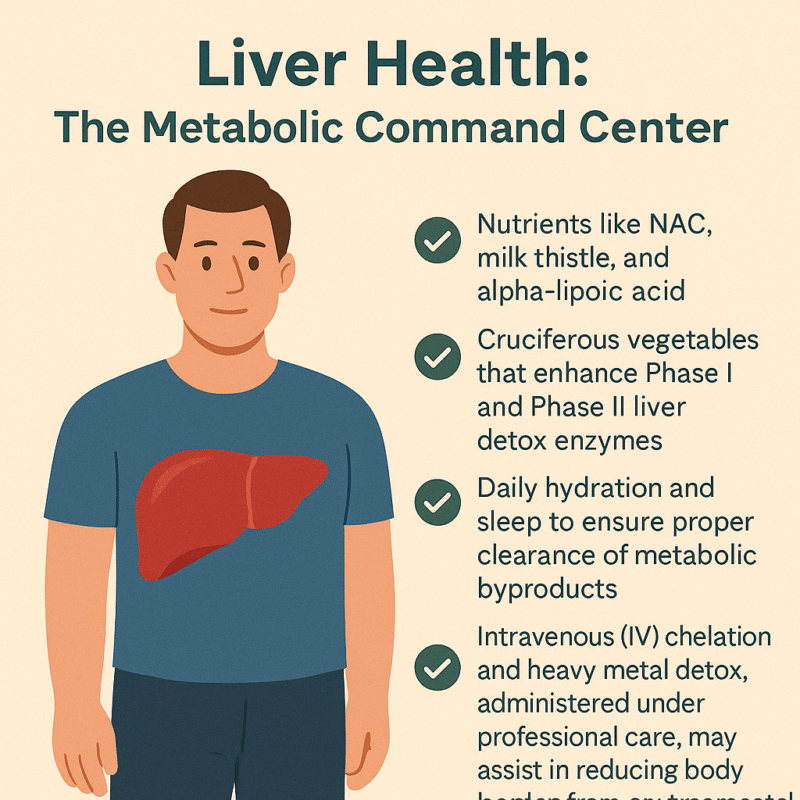
Liver Health: The Metabolic Command Center
Often overlooked in weight loss conversations, the liver plays a truly central role in regulating metabolism, hormone balance, detoxification, and fat processing. It is the body’s metabolic command center, coordinating an astonishing number of chemical reactions every day—more than 500 in total. From metabolizing carbohydrates and breaking down fats to neutralizing toxins and converting hormones, the liver is integral to maintaining internal balance. When the liver is sluggish or overburdened—due to poor diet, excessive alcohol, prescription drugs, or environmental toxins—its ability to process fats and regulate glucose declines. This dysfunction can create a metabolic bottleneck, making weight loss difficult, even in people who are otherwise eating well and exercising.
A compromised liver may allow fatty deposits to accumulate within its own tissue, a condition known as non-alcoholic fatty liver disease (NAFLD). NAFLD is now one of the most common liver conditions worldwide and is strongly associated with insulin resistance, metabolic syndrome, and central obesity [14]. As the liver struggles to detoxify and process nutrients efficiently, inflammation and oxidative stress can build up systemically, impairing not just fat loss but also energy levels, immune function, and hormonal health. Since the liver also helps metabolize estrogens and other steroid hormones, a sluggish liver can worsen estrogen dominance or hormonal imbalance, especially during perimenopause and andropause.
Supporting liver function is thus not just helpful—it is essential for healthy, sustainable weight management. A multipronged approach is best. Certain nutraceuticals are well-researched for their liver-protective properties. N-acetyl cysteine (NAC) boosts intracellular glutathione, the body’s master antioxidant, helping neutralize free radicals and support Phase II detoxification. Milk thistle (silymarin) has been shown to stabilize liver cell membranes and stimulate protein synthesis in hepatocytes, while alpha-lipoic acid supports both liver regeneration and insulin sensitivity [14]. These compounds create a protective biochemical environment that enhances fat metabolism and reduces oxidative damage.
Diet also plays a major role in liver health. Cruciferous vegetables—like broccoli, cauliflower, Brussels sprouts, and kale—are rich in glucosinolates, which stimulate Phase I and Phase II detox enzymes in the liver. These enzymes help convert lipophilic toxins into water-soluble forms that can be safely excreted [15]. The fiber in these vegetables also supports gut-liver axis function by binding toxins and facilitating regular elimination. Combined with sufficient hydration and deep, restorative sleep, these practices help ensure that the liver can efficiently clear metabolic byproducts and prevent the recirculation of toxins in bile.
In more complex or toxin-burdened individuals, intravenous (IV) detoxification strategies may be warranted. Chelation therapy, using agents like EDTA or N acetyl cycteine, under medical supervision, can assist in binding and removing heavy metals such as lead, mercury, and cadmium—substances known to impair mitochondrial function and enzyme activity in the liver. These toxins, when left unchecked, contribute not only to fatty liver and oxidative stress but also to hormonal disruption and sluggish metabolism. Regular assessments and guided detox protocols can significantly reduce this toxic load, often resulting in better energy, improved body composition, and enhanced clarity of mind.
By treating the liver as the metabolic powerhouse that it is, and not merely a silent filter, we create the internal conditions for real transformation. A well-functioning liver clears the path for hormone balance, inflammation reduction, effective fat burning, and ultimately, sustainable weight loss from the inside out.
Brain and Joint Health: Weight Loss Without the Cost
In the pursuit of rapid weight loss, it’s easy to focus exclusively on calories, exercise, and appearance—yet often forgotten are the two pillars of long-term vitality and quality of life: the brain and the joints. Unfortunately, overly aggressive caloric restriction or nutrient-poor diets can have unintended consequences that affect these critical systems. When the body is deprived of key macronutrients and micronutrients, it may cannibalize structural proteins, reduce neurotransmitter synthesis, and accelerate cartilage breakdown. The result? Cognitive fog, mood instability, and increased joint pain—symptoms that are not only discouraging but can derail even the most well-intentioned weight management plans.
The brain is metabolically demanding, consuming over 20% of the body’s energy at rest. It depends on a continuous supply of healthy fats, particularly long-chain omega-3 fatty acids (EPA and DHA), stable glucose levels, and micronutrients like B vitamins, magnesium, and antioxidants to maintain its functions—memory, mood regulation, focus, and neuroplasticity. Erratic blood sugar levels, inflammation, and oxidative stress can impair synaptic efficiency and neurotransmitter production, contributing to fatigue, depression, and anxiety. Similarly, joints require structural proteins such as collagen, as well as synovial fluid support from compounds like hyaluronic acid and methylsulfonylmethane (MSM) to stay resilient under mechanical load, especially during weight-bearing exercises.
To support both neurological and musculoskeletal systems during weight loss, a foundational approach includes ensuring sufficient intake of omega-3 fatty acids, particularly EPA and DHA, which are vital for neuronal membrane fluidity and the regulation of inflammation in both the brain and joints [16]. These fatty acids not only protect against neurodegeneration but have been shown in studies to improve mood, reduce anxiety, and support executive function. For those with dietary restrictions, high-quality fish oil or algae-based omega-3 supplements can provide these benefits with minimal caloric burden.
Incorporating low-impact, joint-friendly movement—such as swimming, yoga, Pilates, or brisk walking—provides the dual benefit of stimulating circulation and maintaining mobility without excessive mechanical strain. This movement also supports lymphatic drainage, which is essential for clearing inflammatory metabolites that can accumulate with tissue breakdown or detoxification.
One underappreciated but powerful ally in preserving both cognitive clarity and joint integrity is pregnenolone, a neurosteroid produced in the brain and adrenal glands. As the precursor to key hormones like DHEA, progesterone, testosterone, and cortisol, pregnenolone plays a central role in neuroendocrine balance. It modulates receptors such as GABA and NMDA, contributing to enhanced mood stability, reduced anxiety, and sharper mental performance. Additionally, some emerging research suggests that pregnenolone may influence connective tissue metabolism and joint resilience, potentially improving recovery and reducing pain perception during periods of weight loss and increased physical demand. By supporting neurohormonal homeostasis, pregnenolone can be a valuable tool for avoiding burnout and breakdown while pursuing body recomposition.
When weight loss is approached through a lens that honors the interconnectedness of brain and joint health, the result is a more sustainable, energizing, and empowering journey. Rather than sacrificing cognitive vitality and physical freedom, we can build a path to health that enhances both—allowing us to think, move, and feel better at every stage of transformation.
Mitochondria: Engines of Life
At the cellular level, weight management is mitochondrial management. These tiny, double-membraned organelles serve as the energy factories of our cells, converting nutrients into usable energy in the form of ATP through oxidative phosphorylation. Their efficiency—or lack thereof—directly dictates how well we burn fat, respond to stress, regulate inflammation, and maintain physical stamina. Impaired mitochondrial function doesn’t just lead to fatigue—it lies at the heart of insulin resistance, obesity, neurodegeneration, and accelerated aging [18]. In essence, when mitochondria fail, the whole body slows down—metabolically, cognitively, and immunologically.
Mitochondria do far more than produce energy; they also regulate apoptosis (programmed cell death), modulate the production of reactive oxygen species (ROS), and participate in the cellular stress response. In individuals with metabolic dysfunction, these mitochondria may become swollen, leaky, and inefficient—burning fuel poorly while spilling oxidative byproducts into the surrounding tissue. This “leaky battery” state can lead to a vicious cycle of inflammation, hormonal disruption, and impaired detoxification, all of which sabotage fat loss and degrade overall vitality. A sluggish mitochondrion doesn’t just stall your metabolism; it creates a state of biological inertia.
Optimizing mitochondrial function is therefore a cornerstone of sustainable weight loss, especially for individuals suffering from fatigue, brain fog, or metabolic resistance. One of the most exciting and non-invasive methods for enhancing mitochondrial health is red and near-infrared light therapy. By stimulating cytochrome c oxidase in the mitochondrial electron transport chain, photobiomodulation boosts ATP output, reduces inflammation, and can even trigger mitochondrial biogenesis—the creation of new mitochondria [19]. This makes red light therapy particularly valuable for those with sedentary lifestyles, injuries, or chronic pain who may not yet tolerate vigorous exercise.
Nutritional and nutraceutical interventions also play a powerful role in mitochondrial revitalization. Key compounds such as Coenzyme Q10 (CoQ10), PQQ, and L-carnitine work synergistically to enhance mitochondrial energy output, protect against oxidative damage, and shuttle fatty acids into mitochondria for oxidation. Among these, methylene blue is gaining interest as a novel “electron cycler”—acting as a bypass for damaged segments of the electron transport chain. By accepting and donating electrons, methylene blue improves redox cycling, enhances ATP production, and reduces ROS generation in compromised cells [20]. Used in microdoses, it has shown promise in conditions ranging from mitochondrial myopathy to cognitive decline, and could serve as a valuable tool in resistant weight loss and energy optimization strategies.
High-dose riboflavin (vitamin B2) and niacin (vitamin B3) offer additional mitochondrial support by functioning as precursors to FAD+ and NAD+, respectively—critical cofactors in enzymatic reactions that drive energy metabolism. These nutrients can be particularly helpful in individuals with mitochondrial fatigue, chronic illness, or those exposed to high levels of environmental toxins. Enhancing the NAD+/NADH ratio, a key marker of mitochondrial health, also promotes autophagy and DNA repair, further linking these vitamins to longevity pathways.
An often-underestimated ally in mitochondrial wellness is ascorbic acid (vitamin C). While best known as an antioxidant, vitamin C also plays a cofactor role in carnitine synthesis, collagen production (crucial for mitochondrial membrane integrity), and several steps within the TCA cycle, the energy-producing hub of the mitochondrion. Its antioxidant properties help buffer against mitochondrial-generated ROS, while also supporting adrenal function during periods of metabolic stress.
Lifestyle strategies round out the mitochondrial toolbox. Cold exposure, intermittent fasting, and high-intensity exercise all stimulate mitochondrial biogenesis and autophagy, creating a cellular environment optimized for fat burning and longevity [21]. Fasting in particular activates AMPK and PGC-1α, key regulators of energy balance and mitochondrial renewal, while simultaneously reducing insulin and inflammation.
When mitochondria thrive, the body gains the capacity to lose fat without losing energy, to detoxify without exhaustion, and to age without decline. By nourishing these intracellular engines, we ignite a foundation not only for sustained weight management, but also for vibrant, whole-body health.
Hormones: Conductors of Weight and Wellness
Hormones are the body’s master messengers, orchestrating nearly every physiological process, from metabolism and mood to sleep, libido, and fat storage. In the context of weight management, hormonal balance is not optional—it is foundational. Hormones act like conductors of a symphony: when in harmony, the body hums along with vitality and metabolic clarity; when imbalanced, even the best efforts in nutrition and exercise may falter. Key players like thyroid hormones, cortisol, insulin, estrogen, and testosterone form a dynamic web. A disturbance in one arm of this network often causes ripple effects across the entire system, creating a cascade of dysfunction that leads to stubborn fat gain, fatigue, mood swings, and muscle loss.
The thyroid gland, for instance, regulates basal metabolic rate through hormones T3 and T4. Suboptimal thyroid function—whether due to nutrient deficiencies (like iodine or selenium), autoimmunity, or stress—can significantly reduce calorie burn and slow fat oxidation, even when diet and activity levels are on point [22]. Without proper thyroid signaling, individuals often experience cold intolerance, constipation, and weight gain despite caloric restriction. Supporting thyroid health requires a blend of nutritional sufficiency, gut health, and in some cases, fine-tuning of T3/T4 balance through medical therapy.
Cortisol, the stress hormone, is equally influential. While short-term cortisol spikes can help mobilize energy during stress or fasting, chronic elevation due to unresolved psychological stress, poor sleep, or overtraining can promote abdominal fat storage, suppress thyroid function, and worsen insulin resistance. Modulating cortisol naturally through lifestyle adjustments—such as breathwork, circadian rhythm alignment, and emotional regulation—is powerful. The inclusion of adaptogenic herbs like ashwagandha and Rhodiola rosea has shown to buffer the physiological effects of chronic stress, enhancing resilience while supporting adrenal recovery [23].
Sex hormones such as testosterone and estrogen also play vital roles. In both men and women, low testosterone is associated with increased fat mass and decreased lean muscle. Estrogen, while often vilified, is essential for bone density, glucose regulation, and mitochondrial function. Hormonal imbalances during menopause, andropause, or due to environmental xenoestrogens can shift body composition unfavorably. In cases of clinically confirmed deficiency or dysfunction, bioidentical hormone replacement therapy (BHRT)—tailored to individual needs and monitored closely—can restore physiological balance, improve metabolic flexibility, and enhance quality of life [24].
Ultimately, hormonal optimization is not about manipulating a single hormone in isolation. It’s about understanding the interdependence of systems—the thyroid talking to the adrenals, the pancreas influencing the ovaries, and so forth. A functional medicine approach uses labs, symptom tracking, and lifestyle factors to address root causes and restore rhythm to the body’s hormonal symphony.
Detoxification: Your Weight Loss Accelerator
In today’s world, toxic burden is a hidden variable in many cases of resistant weight loss. From pesticides and plastics to heavy metals and hormone-disrupting chemicals, we are constantly exposed to substances that the body must metabolize and clear. Many of these toxins are lipophilic, meaning they are stored in fat tissue. As the body burns fat during weight loss, these toxins are released back into circulation. Without adequate support, this process can overwhelm detoxification pathways, resulting in fatigue, brain fog, stalled progress, or even hormone disruption.
Detoxification is not just a cleanse—it’s a biochemical process, primarily performed by the liver, gut, kidneys, skin, and lymphatic system. The liver’s Phase I and Phase II detox enzymes transform fat-soluble toxins into water-soluble metabolites that can be excreted through bile or urine. However, this process requires sufficient cofactors such as sulforaphane (from broccoli sprouts), glutathione, B vitamins, and amino acids like glycine and cysteine [25]. If these nutrients are lacking—or if Phase II is sluggish while Phase I is overactive—intermediary toxins can accumulate, increasing oxidative stress and inflammation.
Supporting detox is a layered endeavor. Consuming cruciferous vegetables, berries, and high-fiber foods provides both enzymatic activation and toxin-binding capacity in the gut. Hydration and adequate bile flow (supported by bitters or phosphatidylcholine) are essential for flushing waste through the liver-gallbladder-intestinal axis. Moreover, regular infrared sauna therapy can augment toxin clearance through the skin, while simultaneously stimulating heat shock proteins that protect cellular integrity [26].
The gut, often referred to as the “second liver,” plays a key role in toxin recycling. A compromised intestinal lining can allow enterohepatic recirculation—the reabsorption of bile-bound toxins—further burdening the liver. Maintaining gut integrity with probiotics, immunoglobulins, and fiber reduces this loop and ensures toxins are carried out effectively [27]. Additionally, movement practices such as rebounding, lymphatic massage, and walking support the drainage systems that move cellular waste out of the body.
For individuals with elevated toxic exposure—such as mold, mercury, lead, or persistent organic pollutants—deeper interventions may be required. IV chelation, phospholipid exchange, and high-dose antioxidant IV therapy can accelerate removal of these compounds when performed under professional care. These therapies help to restore mitochondrial and hormonal function by removing the underlying biochemical irritants that interfere with cell signaling and energy production.
Rather than relying on fads or quick cleanses, a structured, nutrient-dense, and practitioner-guided detox protocol aligns with how the body is biologically designed to heal. In the context of weight loss, it allows for the safe release of stored toxins, reducing inflammatory backlash and preserving hormonal and mitochondrial resilience. Done correctly, detoxification becomes not just a side strategy, but a catalyst for deep metabolic renewal.
The EBOO Advantage: Ozone for Metabolism
In the quest to optimize metabolism, reduce inflammation, and support cellular renewal, Extracorporeal Blood Oxygenation and Ozonation (EBOO) has emerged as a promising adjunctive therapy within integrative and functional medicine. This cutting-edge technique involves drawing blood from the patient, infusing it with a carefully calibrated concentration of ozonated oxygen, and reintroducing it into the body in a closed-loop system. The goal is to stimulate a cascade of oxidative preconditioning responses—essentially “training” the body to bolster its antioxidant defenses, optimize circulation, and enhance mitochondrial resilience. Though still considered investigational in many countries, early studies and clinical observations suggest that EBOO may have multi-system benefits, particularly for individuals dealing with metabolic dysfunction, chronic inflammation, or toxic burden [28].
One of the most compelling aspects of EBOO is its impact on systemic inflammation, which lies at the root of obesity, type 2 diabetes, cardiovascular disease, and autoimmune conditions. By modulating cytokine levels, particularly pro-inflammatory markers like IL-6 and TNF-α, EBOO has demonstrated the potential to lower the inflammatory burden associated with metabolic syndrome [29]. In individuals who have plateaued in their weight loss journey or present with persistent fatigue, brain fog, or joint pain—despite lifestyle interventions—EBOO may offer a way to reduce subclinical inflammation and restore metabolic momentum. Its potential to support immune recalibration without immunosuppression makes it uniquely suited for conditions marked by immune overactivity and oxidative stress.
Another key benefit of EBOO lies in its support for mitochondrial function. By improving oxygen delivery to tissues and enhancing redox balance, ozone therapy may help optimize aerobic respiration, leading to improved energy production, clearer thinking, and greater endurance [30]. Ozone is thought to upregulate antioxidant systems such as superoxide dismutase (SOD) and glutathione peroxidase, which counteract the reactive oxygen species generated during fat metabolism and detoxification. This makes EBOO particularly valuable when paired with weight loss, as the release of toxins from fat cells can temporarily increase oxidative stress. By boosting the body’s adaptive antioxidant response, EBOO creates a smoother metabolic transition and reduces detox-related fatigue.
Safety remains paramount. While ozone therapy has been used for decades in parts of Europe, it requires precise dosing and delivery techniques to avoid oxidative overload or complications. EBOO, unlike direct intravenous ozone (DIV), allows for controlled, high-volume exposure in a filtered circuit, minimizing the risk of gas embolism or localized irritation. It must be administered by trained clinicians using medical-grade ozone generators and ozone-resistant materials. As with any emerging therapy, patients should undergo appropriate screening for contraindications, such as G6PD deficiency or unstable cardiovascular conditions, and engage in shared decision-making with their providers.
Though more randomized controlled trials are needed to validate EBOO’s long-term efficacy, early results and clinical experience are encouraging. For individuals seeking to enhance metabolic recovery, reduce inflammation, and support detoxification in the context of structured weight loss programs, EBOO may offer a novel and systemically restorative tool. When integrated with nutrition, movement, mitochondrial support, and hormone balancing, ozone therapy can become part of a multi-layered strategy for true metabolic renewal.
A New Metric of Success: Beyond BMI
For too long, weight management has been reduced to a single, overly simplistic number: Body Mass Index (BMI). While easy to calculate, BMI fails to distinguish between muscle and fat, visceral versus subcutaneous adiposity, or inflammation versus metabolic health. It tells us nothing about bone density, hormonal patterns, micronutrient status, or mitochondrial vitality. And most importantly, it tells us nothing about how someone feels—their energy, clarity, strength, or resilience. In our effort to measure health, we’ve often confused simplicity with accuracy.
True transformation goes far beyond weight or BMI. The real markers of meaningful, lasting change are found in deeper metrics: inflammatory markers like hs-CRP and IL-6, fasting insulin, lean muscle retention, DEXA-assessed bone density, and hormonal balance across the adrenal-thyroid-gonadal axis. It includes the quality of one’s sleep, the stability of energy throughout the day, the sharpness of thought, and the ease of movement. These are the dimensions where real health lives—and where future weight loss strategies must focus.
Perhaps the most powerful of all is metabolic flexibility—the ability to switch between burning fat and glucose based on energy demand and availability. A metabolically flexible body can fast without crashing, exercise without bonking, and enjoy whole foods without guilt. It’s not enslaved by cravings or bound to rigid macros. Instead, it adapts with grace to the changing needs of life. Cultivating this flexibility requires muscle preservation, mitochondrial efficiency, hormonal balance, and a nutrient-dense, anti-inflammatory lifestyle—not endless restriction or willpower.
This shift in focus—from mere weight to whole-system performance—is not just empowering, it’s necessary. It invites both patients and practitioners to ask new questions: Are we building strength or just losing mass? Are we reducing inflammation or just chasing numbers? Are we nourishing longevity or just shrinking temporarily? With better questions come better answers—and ultimately, better outcomes.
Final Thoughts: The Future of Weight Loss
As we move into a more advanced, personalized, and integrative era of medicine, our understanding of weight must also evolve. Weight is not a standalone symptom, but rather a visible expression of complex physiological imbalances involving hormones, detoxification, gut health, mitochondrial performance, circadian biology, and neuroendocrine integrity. To treat weight loss effectively is to treat the body as an ecosystem—dynamic, interconnected, and responsive to its environment.
In the future, lean muscle will be viewed not merely as aesthetic but as a vital organ of longevity and metabolic defense. Mitochondria, once relegated to cell biology lectures, will become clinical biomarkers, monitored and supported through light, nutrients, and precision medicine. Liver health will no longer be secondary but central to fat metabolism, hormonal processing, and detox resilience. Hormonal intelligence will replace hormonal fear, recognizing the power of estrogens, androgens, cortisol, and thyroid in shaping both physical composition and psychological health.
Inflammation will be addressed not with blanket suppression but with targeted, nuanced interventions—from resveratrol and curcumin to ozone and red light—each chosen to recalibrate rather than mute. Technologies like EBOO therapy, IV detox, and advanced nutritional protocols will integrate with behavioral science and emotional healing to create approaches that are both rooted in science and personalized for the individual.
For patients, this is a call to redefine success. Success isn’t how much you weigh; it’s how well you live in your body. It’s waking up energized, thinking clearly, digesting easily, and moving freely. It’s having a body that works with you, not against you, in all seasons of life.
For practitioners, it’s a reminder that the future of medicine lies not just in more data, but in deeper systems thinking—seeing how the thyroid speaks to the mitochondria, how detox affects estrogen metabolism, how cortisol reshapes the gut lining. It is a practice of artful precision, where diagnostics and lifestyle medicine meet.
Whether you’re a patient seeking a new path or a doctor crafting a new protocol, know this: Real weight management is not a sprint—it’s a symphony. It is the orchestration of metabolism, movement, nourishment, and nervous system balance. Every pound lost wisely is not just fat gone—it is years gained in strength, clarity, and resilience. This is not weight loss for the mirror. This is transformation for life.
Written by: [Dr. Mitra Basu Chhillar]
Functional Medicine Advocate | Metabolic Health Educator
References
- Cruz-Jentoft AJ, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39(4):412-23.
- DeFronzo RA, et al. Pathogenesis of type 2 diabetes mellitus. Med Clin North Am. 2004;88(4):787–835.
- Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8(8):457–65.
- Phillips SM. Nutrient-rich meat proteins in muscle maintenance and function. Br J Nutr. 2012;108(Suppl 1):S51-3.
- Churchward-Venne TA, et al. Nutritional regulation of muscle protein synthesis with resistance exercise. Nutr Metab (Lond). 2012;9:40.
- Villareal DT, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011;364(13):1218–29.
- Karsenty G, Ferron M. The contribution of bone to whole-organism physiology. Nature. 2012;481(7381):314–20.
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–81.
- Blake GM, et al. Bone mineral density and DEXA. Bone. 2007;41(4):548–56.
- Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860–7.
- Esser N, et al. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract. 2014;105(2):141–50.
- Patel SR, et al. Short sleep duration and weight gain. Sleep. 2006;29(2):195–200.
- Baur JA, Sinclair DA. Therapeutic potential of resveratrol: the in vivo evidence. Nat Rev Drug Discov. 2006;5(6):493–506.
- Sutti S, Albano E. Adaptive immunity: an emerging player in the progression of NAFLD. Nat Rev Gastroenterol Hepatol. 2020;17(2):81–92.
- Higdon JV, Frei B. Cruciferous vegetables and human cancer risk: epidemiologic evidence and mechanistic basis. Pharmacol Res. 2007;55(3):224–36.
- Dyall SC. Long-chain omega-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA and DHA. Front Aging Neurosci. 2015;7:52.
- Bello AE, et al. Collagen hydrolysate for the treatment of osteoarthritis and other joint disorders: a review. Curr Med Res Opin. 2006;22(11):2221–32.
- Petersen KF, et al. Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science. 2003;300(5622):1140–2.
- Hamblin MR. Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochem Photobiol. 2018;94(2):199–212.
- Gonzalez-Lima F, Auchter AM. Methylene blue as a cognitive enhancer. Metab Brain Dis. 2015;30(3):593–9.
- Mattson MP, et al. Intermittent metabolic switching, neuroplasticity and brain health. Nat Rev Neurosci. 2018;19(2):63–80.
- Zimmermann MB, Boelaert K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015;3(4):286–95.
- Panossian A, Wikman G. Effects of adaptogens on the central nervous system and the molecular mechanisms associated with their stress-protective activity. Pharmaceuticals. 2010;3(1):188–224.
- Holtorf K. Hormone replacement therapy and the prevention of aging. Postgrad Med. 2009;121(1):73–85.
- Pizzorno J. Environmental toxins and detoxification. Integr Med (Encinitas). 2014;13(1):8–14.
- Hannuksela ML, Ellahham S. Benefits and risks of sauna bathing. Am J Med. 2001;110(2):118–26.
- DeMeo MT, et al. Intestinal permeability defect in irritable bowel syndrome: a pilot study. Neurogastroenterol Motil. 2002;14(6):669–75.
- Bocci V. Ozone: A New Medical Drug. Dordrecht: Springer; 2011.
- Elvis AM, Ekta JS. Ozone therapy: A clinical review. J Nat Sci Biol Med. 2011;2(1):66–70.
- Martínez-Sánchez G, et al. Therapeutic properties of ozone in patients with diabetes mellitus. Diabetes Metab Syndr. 2010;4(2):113–7.
Leave a Reply