Premenstrual syndrome, premenopause and menopause : women keep suffering silently
But is suffering limited to women?

Introduction to Premenopausal Syndrome and Premenstrual Syndrome (PMS)
The journey through womanhood is marked by various physiological milestones, with premenopausal syndrome and Premenstrual Syndrome (PMS) significantly impacting many women’s lives. Scientific studies and publications have shed light on these conditions, offering insights into their symptoms, treatment, and the hormonal dynamics at play.
Premenstrual Syndrome (PMS) and Premenstrual Dysphoric Disorder (PMDD) have been recognized for their substantial impact on the luteal phase of the menstrual cycle, characterized by both physical and psychiatric symptoms. These conditions significantly affect women’s lives, leading to a search for effective treatments ranging from hormonal therapy to lifestyle adjustments and herbal remedies.
The pathophysiology of PMS has been linked to hormonal changes following ovulation, with symptoms not tied to specific hormone levels but rather to the response of the body to these hormonal shifts. The role of progesterone, produced by the ovary, and its metabolites has been highlighted in relation to neurotransmitter function, suggesting a complex interplay between hormones and brain chemistry.
Complementary and alternative medicines, such as Vitex agnus castus, have been explored for their efficacy in treating PMS symptoms. A systematic review and meta-analysis aimed to assess the acceptability and effectiveness of Vitex agnus castus preparations, finding a large pooled effect in placebo-controlled trials. However, the studies included in the analysis showed a high risk of bias and heterogeneity, underlining the need for high-quality research to conclusively determine the benefits of such treatments.
These findings underscore the importance of a nuanced understanding of premenopausal syndrome and PMS, advocating for continued research and evidence-based approaches to treatment. The complexities of hormonal imbalances and their effects on mental and physical health demand a multifaceted strategy, integrating medical, lifestyle, and potentially herbal remedies to support women through these challenging phases of life.
Symptoms and Difficulties Faced by Sufferers

Premenstrual Syndrome (PMS) encompasses a range of somatic and psychological manifestations that occur during the luteal phase of the menstrual cycle, causing substantial distress and functional impairment. These symptoms typically resolve within a few days of menstruation onset. Scientific research highlights that PMS affects a considerable proportion of women of reproductive age, with pooled prevalence rates reaching up to 47.8% worldwide. Symptoms range from changes in appetite and abdominal pain to mood swings and anxiety, significantly affecting daily life and overall health. Furthermore, Premenstrual Dysphoric Disorder (PMDD), a severe form of PMS, is recognized as a psychiatric disorder, underscoring the need for comprehensive treatment approaches, including nonpharmacological and pharmacological interventions.
The prevalence of PMS varies across different regions, with studies reporting rates as low as 12% in France and as high as 98% in Iran. This variability points to the influence of cultural, environmental, and methodological factors in the diagnosis and reporting of PMS symptoms. Despite the challenges in establishing a universal prevalence rate, the trend of increasing PMS awareness and reporting over the years suggests a growing acknowledgment of its impact on women’s health.
In adolescent populations, the prevalence and characteristics of PMS symptoms offer additional insights. A study conducted among school-going girls in Aligarh, Uttar Pradesh, found that 37.7% of participants reported experiencing PMS, with abdominal bloating and social withdrawal being among the most common symptoms. This study also identified several risk factors associated with PMS, including age, education status, and menstrual cycle characteristics, highlighting the complex interplay of biological and sociocultural factors in the manifestation of PMS symptoms.
These findings emphasize the importance of recognizing and addressing PMS and premenopausal symptoms as significant health concerns. Through integrating evidence-based evaluation and treatment strategies, including lifestyle modifications and targeted pharmacotherapy, women can achieve better management of their symptoms, enhancing their quality of life and overall well-being.
Premenopausal Syndrome and Premenstrual Syndrome (PMS), while distinct, share a range of symptoms that significantly impact the daily lives of many women. The transition to menopause, known as perimenopause, can begin years before menopause itself, bringing with it symptoms that are often unpredictable and varied. Premenstrual syndrome, recurring monthly, can also severely disrupt a woman’s emotional and physical well-being.

Emotional and Psychological Impact:
- Mood Swings and Irritability: Many women experience drastic mood swings and irritability, affecting their interpersonal relationships.
- Depression and Anxiety: A significant number report feelings of depression or heightened anxiety, impacting their mental health.
- Concentration Difficulties: The ability to focus and perform mentally intensive tasks can decline, affecting professional life.
Physical Symptoms:
- Cramps and Headaches: These can range from mild to debilitating, often requiring medication.
- Fatigue: Persistent tiredness, despite adequate rest, makes daily activities challenging.
- Bloating and Weight Gain: Fluid retention leads to discomfort and impacts self-esteem.
Premenopausal syndrome sufferers could show symptoms as below.
Physical Symptoms:
- Premenopausal Syndrome: Women in the premenopausal phase may experience irregular periods, hot flashes, night sweats, sleep disturbances, and fatigue. There’s also a noticeable change in libido, vaginal dryness, and discomfort during intercourse.
Emotional and Psychological Symptoms
- Emotional symptoms are profound and often the most challenging aspect of both conditions. Women may experience mood swings, irritability, anxiety, depression, and feelings of overwhelm. There’s also a reported decrease in concentration and a sense of losing control over emotions, leading to tension in personal and professional relationships.
Impact on Daily Life
The intensity of these symptoms can severely disrupt daily activities, work productivity, and social engagements. The unpredictability of symptoms, especially with PMS, means that women often have to modify their plans or commitments at the last minute, leading to stress and a feeling of unreliability.
Coping Mechanisms and Challenges
Many women develop coping mechanisms to manage their symptoms, from dietary changes and exercise to meditation and yoga. However, the efficacy of these strategies can vary, and the search for effective relief is often a process of trial and error, contributing to a sense of frustration and helplessness.
These symptoms represent more than mere inconveniences; they can lead to substantial distress, affecting one’s quality of life.. Despite a high prevalence, a culture of silence often surrounds these conditions. Many women feel embarrassed to discuss their symptoms, fearing judgment or dismissal. The lack of open conversation and education around these topics means that symptoms are often normalized, leading individuals to believe that their discomfort is something to be endured rather than treated. Consequently, many cases remain untreated or are inadequately addressed, with women resigning themselves to silent suffering, unaware of potential avenues for relief.
Hormonal Imbalance: Estrogen and Progesterone
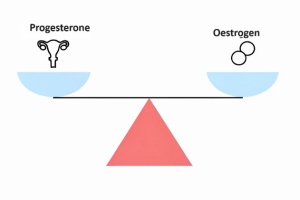
At the heart of PMS and perimenopausal symptoms is a delicate balance between estrogen and progesterone, two key hormones in the female reproductive system. During the menstrual cycle, fluctuations in these hormone levels are normal. However, problems arise when there is an excess of estrogen relative to progesterone, a condition known as estrogen dominance. This imbalance can lead to a myriad of symptoms associated with PMS and the perimenopausal period.
Estrogen dominance can be exacerbated by external factors such as stress, diet, and exposure to xenoestrogens found in certain plastics and chemicals. These factors, combined with the body’s natural hormonal shifts, can lead to an exacerbation of PMS symptoms and increase the difficulties faced during the perimenopausal transition.

Understanding the role of these hormonal imbalances is crucial for addressing the root cause of the symptoms many women face. However, the traditional medical approach to these issues often falls short, relying on symptom management rather than addressing underlying hormonal imbalances.
Ineffectiveness of Traditional Treatment Methods
Traditional treatment methods, including the use of non-steroidal anti-inflammatory drugs (NSAIDs), hormonal contraceptives, and antidepressants, often offer insufficient relief and come with a range of side effects. These treatments may address some symptoms but do not tackle the underlying hormonal imbalance. Moreover, the one-size-fits-all approach of conventional medicine fails to accommodate the individual variability in symptom presentation and severity.
The Role of Low Progesterone in PMS
Low levels of progesterone relative to estrogen can significantly contribute to the development of PMS symptoms. Progesterone plays a crucial role in regulating the menstrual cycle and supporting pregnancy. When progesterone levels are insufficient, it can lead to estrogen dominance, exacerbating PMS symptoms. Natural progesterone supplementation has been shown to mitigate these effects by rebalancing hormone levels, offering a targeted approach to managing symptoms.
Benefits of Natural Progesterone and Administration Methods
Natural progesterone, particularly in micronized form, offers a promising alternative to synthetic hormones. Unlike synthetic progestins, natural progesterone is identical to the hormone produced by the body, minimizing the risk of side effects and promoting better hormone balance. However, oral administration of progesterone can lead to its rapid metabolism in the liver, reducing its efficacy and potentially leading to the production of unwanted metabolites.

Natural progesterone, particularly in micronized form, offers a promising alternative to synthetic hormones. Unlike synthetic progestins, natural progesterone is identical to the hormone produced by the body, minimizing the risk of side effects and promoting better hormone balance. However, oral administration of progesterone can lead to its rapid metabolism in the liver, reducing its efficacy and potentially leading to the production of unwanted metabolites.
Progesterone oil: A Solution

SOMA Progesterone oil, formulated with micronized progesterone from wild yam in medium-chain triglyceride (MCT) oil, represents an innovative approach to hormone supplementation. This formulation enhances the absorption and efficacy of progesterone, offering a natural and effective way to manage PMS and premenopausal symptoms.
Best Practices for Progesterone Oil Usage
For menstruating women, the optimal time to use progesterone oil is from the 14th day of the menstrual cycle for 14 days, mirroring the body’s natural rhythm. Postmenopausal women may benefit from daily use. Application before bed, targeting areas like the forearms, underarms, thighs, and abdomen, ensures optimal absorption and efficacy. However, due to potential anti-testosterone effects, males should avoid exposure to the oil.
Conclusion: Improving Quality of Life with Progesterone Oil

The journey through premenopause and the monthly menstrual cycle can be challenging, but it doesn’t have to be debilitating. Through the strategic use of natural progesterone, particularly in the form of topical SOMA progesterone, women can find relief from the myriad symptoms of PMS and premenopausal syndrome. This approach offers a safe, effective, and tailored method to restore hormonal balance, improve well-being, and reclaim quality of life.
By addressing the root hormonal imbalances with natural progesterone, and applying the latest in absorption technology, SOMA progesterone oil offers a beacon of hope for those navigating the complexities of these conditions. Through informed choices and access to effective treatments, the silent suffering can finally be alleviated, allowing women to lead fuller, more vibrant lives.
References
- Patel S, Homaei A, Raju AB, Meher BR. Estrogen: The necessary evil for human health, and ways to tame it. Biomed Pharmacother. 2018 Jun;102:403-411. doi: 10.1016/j.biopha.2018.03.078. Epub 2018 Mar 22. Review. PubMed PMID: 29573619.
- Bäckström T, Andreen L, Birzniece V, Björn I, Johansson IM, Nordenstam-Haghjo M, Nyberg S, Sundström-Poromaa I, Wahlström G, Wang M, Zhu D. The role of hormones and hormonal treatments in premenstrual syndrome. CNS Drugs. 2003;17(5):325-42. doi: 10.2165/00023210-200317050-00003. Review. PubMed PMID: 12665391.
- Tarannum F, Khalique N, Eram U. Premenstrual syndrome: Prevalence, symptoms, and associated risk factors among adolescent girls in Aligarh, Uttar Pradesh. Indian J Public Health. 2021 Oct-Dec;65(4):396-399. doi: 10.4103/ijph.ijph_985_21. PubMed PMID: 34975086.
- A DM, K S, A D, Sattar K. Epidemiology of Premenstrual Syndrome (PMS)-A Systematic Review and Meta-Analysis Study. J Clin Diagn Res. 2014 Feb;8(2):106-9. doi: 10.7860/JCDR/2014/8024.4021. Epub 2014 Feb 3. PubMed PMID: 24701496; PubMed Central PMCID: PMC3972521.
- Gudipally PR, Sharma GK. Premenstrual Syndrome. 2024 Jan;. PubMed PMID: 32809533.
- Imai A, Ichigo S, Matsunami K, Takagi H. Premenstrual syndrome: management and pathophysiology. Clin Exp Obstet Gynecol. 2015;42(2):123-8. Review. PubMed PMID: 26054102.
- Appleton SM. Premenstrual Syndrome: Evidence-based Evaluation and Treatment. Clin Obstet Gynecol. 2018 Mar;61(1):52-61. doi: 10.1097/GRF.0000000000000339. Review. PubMed PMID: 29298169.
